For the Love of Vulvas
This may seem like a “juicy” and taboo guide, but as an Occupational Therapist, I cannot think of a better topic to discuss approaching Valentine’s Day. Sexual activity is an activity of daily living, just as bathing, toileting, dressing, and eating are. These activities are essential to taking care of our bodies. But before we discuss sex, we should learn some anatomy. Specializing in pelvic health, I have learned a thing or two about what goes on “down there,” so vulva owners this one is for you!
First and foremost. Anatomy.
Do you know what your anatomy “down there” looks like? No two vulvas are alike, so it is important to get to know yours, specifically. Why, you may be wondering? If there are any changes, you will be able to address your concerns with your provider. If you never look, how will you even know if something looks different then before? You may see your gynecologist annually or possibly every three years when your pap smear is due, so it’s important to fill in those gaps with self-checks. So, when you check your boobs (this is your gentle reminder, go check your boobs!), go check “down there.” Grab a mirror, look at your anatomy laying down, sitting, and standing up. What do you see?
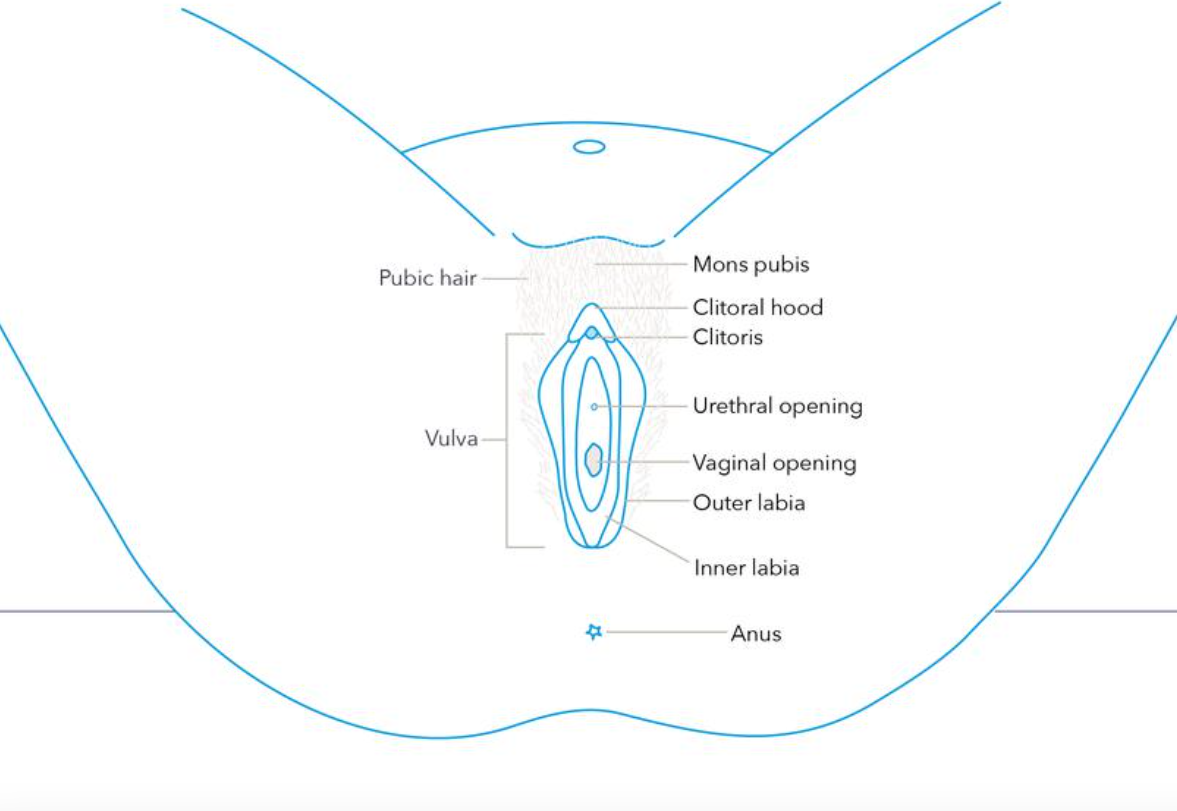
Important things to look at:
Outer labia
Inner labia
Clitoral hood
Vaginal Canal
Perineum
Anus
Do not be alarmed if yours looks different than what you expected to see – it is absolutely fine, and you are uniquely YOU. It’s called vulva diversity!
Here is a picture to help orient you to what you should be looking at. You will have to use somewhat of an imagination since this is not a picture of real-life anatomy.
Self Investigation.
Now that you are ready to take a peak. What are you looking for?
When looking, you want to note any areas of redness, irritation, swelling, changes in coloring, white spots, bumps, lesions, adhesions, or dry skin. Do you have any sensitivity, pain, or pressure in a specific area?
If you have a pelvic floor therapist, they will help address your concerns, and if it’s out of their scope of practice, they may refer you to your gynecologist, a vulvar specialist, or a vulvar dermatologist. So if you have any concerns or questions, leave it to the experts and not search engines.
Vulva Self Check
“Okay, I took a peek. Now what?”
If you want to step away from the clinical investigation, shift gears and get to know your anatomy through pleasurable self-touch. Maybe you are not sure what feels good to your body, how to make it feel good, or maybe none of it feels good and it actually hurts.
By investigating through self touch, you become quite the expert of your own body. As you should be. Leave the shame at the door. This body belongs to you, it is perfectly imperfect and it deserves to feel pleasure not pain. If you do feel discomfort, note where it is felt and how you would describe it. This will help your doctors or therapists better serve you , and help you heal.
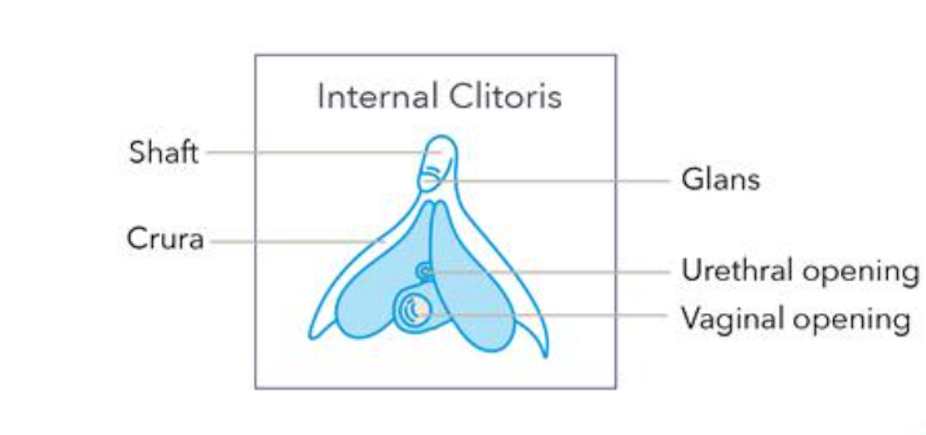
The “Where’s Waldo?” of female anatomy, the Clitoris.
Did you know that when aroused, and blood starts flowing to our genitals, the clitoris becomes erect like a penis? One of the primary functions of the clitoris is for pleasure. The clitoris has just as many nerve endings as a penis, if not more. If that isn’t jaw dropping, I don’t know what is!
It is important to discuss the clitoral hood. Reference back to the video above if needed. Yes your clitoris has a hood, and the hood protects this incredible organ. Your hood should slide and glide with ease. Especially if having an orgasm is something on your radar. If there are any adhesions and it doesn’t move well, this could cause discomfort.
“Instead of the big “O”… I get a big OUCH!”
Sex should never hurt. Period. Yes people may enjoy pain that comes with different fetishes or kinks. That is not what we are discussing here. We are talking about un-invited and unwanted, pain “down there.”
You are not alone and this is common, though not frequently discussed amongst friends and family. Pain does not have to be the norm for you.
Not only does the clitoris have some performance expectations for pain free and pleasurable sexual activity, but the uterus needs to elevate and the vaginal canal needs to expand in order to accept penetration. Our pelvic floor muscles (we have around 16 of them!) need to move through a full range of motion, of contraction and relaxation, for improved pleasure and a more robust orgasm. If your pelvic floor muscles are tight, stuck in a contracted state, or experiencing spasms, this affects that range of motion, impacting pain, and arousal.
Aside from the mechanical aspects of what may be causing pain and discomfort, our body holds onto emotion, and has memory. If you have been feeling stressed, anxious, have experienced a traumatic event (big, small, or maybe something that happened in childhood), have a hormonal imbalance, etc., this can impact how our body feels and performs. This inhibits our ability to enter a parasympathetic state where our nervous system calms down, including calming our muscles down.
Are you clenching your jaw? Did you know that your jaw can impact your pelvic floor? If you release tension in your jaw, it will help release some tightness in your pelvis, as well as your back, and sacral region. In a follow up article, we will dive deeper into mobility work that helps lengthen and relax your pelvic floor muscles, as a preparatory step and recovery phase to sexual intimacy. Stay tuned for an announcement on a release date!
If pain free and pleasurable sex seems out of reach at the moment, or if you experience fear or pain with any penetration, such as with a finger, with tampon insertion, or during an internal gynecological exam, know that there is hope and help available. Pelvic health therapists help peel back the onion, uncovering layers of what is truly going on, using a biopsychosocial approach. This helps discover the root cause to begin a healing journey, together.
Intimacy is a marathon, not a sprint.
Women need approximately 40 minutes of foreplay to feel aroused. 40 minutes can be a long time, and requires some patience, especially if your partner is already “in the mood”. With that being said, it’s important to note that lubrication is not an indication of desire. Just because you are lubricated, does not mean you are in the mood and that your body is ready for intimacy. Similarly, just because you are not lubricated, does not mean you are not in the mood.
If you track patterns in your menstrual cycle, you may notice more or less discharge/fluid, and even different consistencies, at different times of the month. This is different from arousal fluid.
Life, stress, hormones, trauma, and medications, all impact our natural lubrication process. It becomes something our body does NOT prioritize; and that is OKAY! Also, as we get older, the integrity of our vaginal walls become thinner, and with hormonal changes we may in fact be, drier.
What we do know, is that lubrication helps protect the vaginal lining. Thankfully there are some great lubricants available. There are quite a few out there, so it’s important to read ingredients. Some ingredients can cause an increase in irritation/infections. One quick example is glycerin, a sugar alcohol, which can lead to yeast overgrowth. When we dive into eating for vaginal health at a later date, you will learn that increased sugars in our diet (like glucose) also can lead to a yeast overgrowth! What goes in and on our body truly matters!
Different from lubrication, there is a possibility you may need a vaginal moisturizer/vulva cream, and that is something you can talk to your gynecologist about.
For more specifics on lubrications, I have included 2 well thought-out and researched pieces by Pelvic Health Occupational Therapists that I have met, and learned from, over the past few months. The 1st link below is to an article, and the 2nd link below is to a video.
Thank you for taking the time to read my guide to a vulva introduction you didn’t know you needed. Maybe something resonated with you and maybe you took away some knowledge that you didn’t have before. Let’s normalize the conversation, and talk more openly about what is going on “down there.”
There is so much more to discuss, so stay tuned for more learning opportunities to improve your pelvic health and overall wellness!
Yours in pelvic health,
Danielle @ TheraPelvic